Frequently Asked Questions
Plasma is the liquid portion of your blood. Your blood is made up of a liquid portion and a cellular portion. The cellular portion contains white blood cells that fight infection, red blood cells that carry oxygen, and platelets that aid clotting. Plasma is the liquid portion of your blood. It contains proteins and antibodies, which are produced by the immune system to fight diseases. Plasmapheresis is a blood donation process in which you donate only the liquid or plasma portion of your blood. The cellular portion of your blood is separated from the plasma by an automated instrument that is approved by the Food and Drug Administration (FDA). As part of this same automated process, the cellular portion is returned to you and the liquid plasma portion is collected.
To donate plasma, you must be a healthy individual at least 18 years of age or older, weigh at least 110 pounds, have a valid ID and pass all other required donor eligibility criteria including a physical exam and screening for infections. Following a well-balanced diet and drinking plenty of water before donating is also recommended.
Donating plasma is a very safe procedure with minimal or no side effects. On your initial visit, and annually, you will receive a physical exam and your medical history will be recorded. These steps help ensure donating is safe for you and protect the recipient of the therapies made from your plasma. On subsequent visits, we will check your vital signs and ask some questions about your health since your last donation. In addition, your hematocrit (the percentage of blood volume occupied by red blood cells) and plasma protein levels will be measured.
All collection supplies that come in contact with your blood are single use only and are discarded and replaced with new, sterile materials each time a donation procedure is performed. All of our procedures are approved by the Food and Drug Administration (FDA), as well as various European certifications, under strict guidelines.
Our staff is dedicated to making your visit comfortable. You can spend the donation time relaxing, watching television, surf the internet, read your favorite magazine or book.
Through a process called Plasmapheresis. This is a process in which you only donate the liquid portion of your blood, the plasma. It is separated from the cellular portion of your blood by an automated instrument that is approved by the Food and Drug Administration (FDA). As part of this same automated process, the red blood cells are returned to you and the liquid portion, the plasma, is retained in a special collection container. By receiving your red cells back, you should not feel tired as normally associated with donating blood. This process has been around since the 1950’s.
The body replaces the plasma removed during the donation process quickly; therefore, healthy individuals can donate as often as twice a week.
On your first visit, the whole process, including a physical exam and the plasma donation, usually takes about two hours. On subsequent visits, you can anticipate spending a little under one hour at the center.
Southern Blood Services performs extensive screening tests on a sample of every unit of plasma collected. Each donation is thoroughly tested for various infectious agents including Hepatitis B, Hepatitis C and HIV.
The plasma that is collected at Southern Blood Services is manufactured into a wide variety of life-saving products that benefit thousands of people everyday. Plasma is used in the treatment of serious disorders such as immune system deficiencies and prevents diseases like Hemolytic Disease of the Newborn; in fact each donation produces 40 RhoGam® or RhO(D) immune globulin shots.
In addition, hospitals and blood centers use plasma based products to type and screen other people’s blood for transfusions and organ transplants.
It is important to remember that plasma is not a substance that can be produced in a laboratory or some other artificial environment. It can only be obtained from healthy adults. When you donate plasma, you are helping to save lives.
Donating plasma can be one of life's most enriching experiences. Aside from the knowledge that you have helped others with your plasma, you will receive monetary compensation for your time if you qualify for a program.
SBS is certified by and complies with requirements from the following:
- Food and Drug Administration (FDA)
- State of Alabama
- State of Tennessee
- Plasma Protein Therapeutics Association (PPTA)
- International Quality Plasma Program (IQPP)
- Clinical Laboratories Improvement Amendment (CLIA)
- Occupational Safety and Health Administration (OSHA)
If you have an antibody, we are willing to work with you. We currently have three collection sites but also a vast network of other centers that may be willing to do the collection process. In special circumstances it is even possible to fly you to one of our centers at our expense. As each case is unique, we encourage you to contact us to further information.
The Rh factor is the “+” (Positive) or “=” (Negative) after your blood type (A, B, AB, or O). This means your blood type is negative (A-, B-, O- or AB-) and you don’t have a protein on the surface of your red blood cell. Rh positive (A+, B+, O+ or AB+) would mean that you do have that protein. "Rh-negative" and "Rh-positive" are really just terms that further define what type of blood a person has, beyond the general blood type A, B, O, and AB.
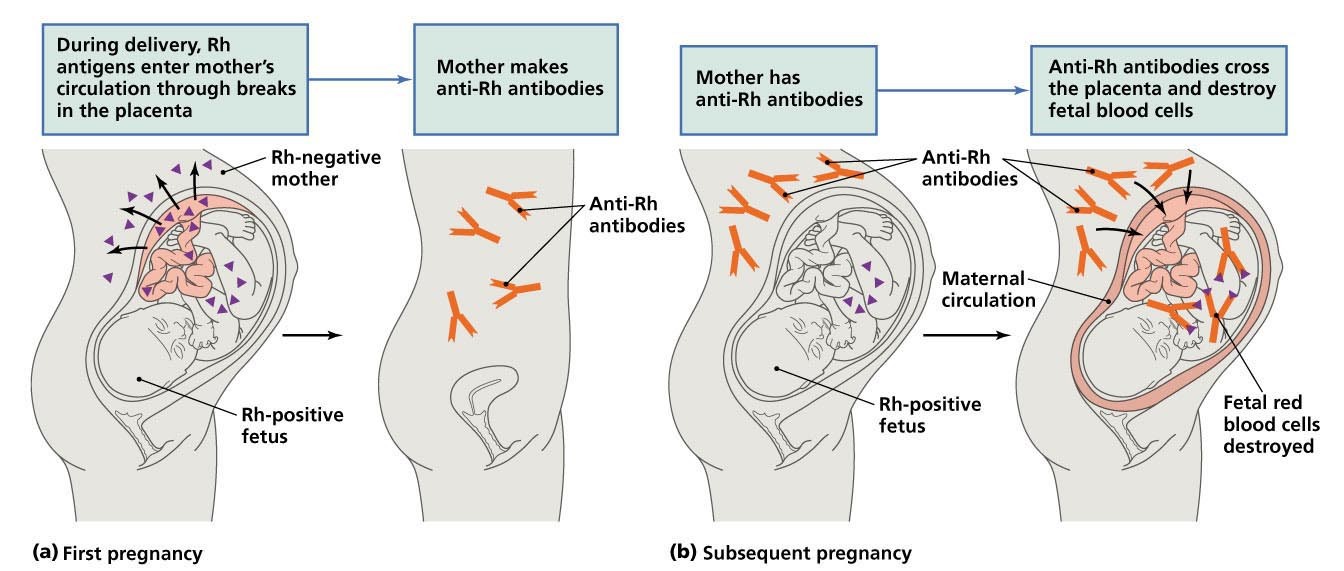
Being Rh-negative is neither good nor bad, but it can be serious issue if you're pregnant by or planning to have a child with a man who is Rh-positive. If you're Rh-negative and carrying a baby who is Rh-positive (like the baby’s father), your immune system, which fights off invaders to keep you healthy, will recognize your baby's Rh-positive red blood cells as foreign to your Rh-negative blood and will begin producing antibodies intended to destroy your baby's blood cells. If it is your first pregnancy, chances are everything will be fine. These crusading antibodies usually are not dangerous until subsequent pregnancies, when they've had time to grow in strength and number. This is why you have to worry about future pregnancies. Once the antibodies begin attacking, they can lower a baby's red blood cell count, which can lead to jaundice, anemia, mental retardation or heart failure. In the most severe cases, it can be fatal in utero (during pregnancy) or shortly after delivery. This condition is known as Hemolytic Disease of the Newborn, and for Rh-negative women, all future pregnancies are at risk. Fortunately, treatment can virtually eliminate the risk.
An antibody is a protein made by your body. Antibodies usually bind to foreign substances, such as bacteria and viruses, and destroy them. A red blood cell antibody is one that “attacks” red blood cells. Your red blood cells have certain “markers” on them, called antigens. If your immune system sees a red blood cell antigen that is “foreign” (such as from a blood transfusion), it will make antibodies to destroy it.
| If your ABO blood type is | Your body will naturally make these antibodies |
| 0 | Anti-A and Anti-B |
| A | Anti-B |
| B | Anti-A |
| AB | None |
For example, if your ABO blood type is “O,” you will have antibodies against types A and B. The Rh factor is another antigen. People who are Rh negative can make antibodies to blood that is Rh positive. When you get a red blood cell transfusion, the transfused blood must be compatible with your ABO and Rh type.
Besides ABO and Rh antigens, there are more than 50 blood group antigens that can be found on the surface of red blood cells. Your body can make red blood cell antibodies to these other blood group antigens if you have:
- Had a blood transfusion in the past (the more transfusions, the more exposure to “foreign” antigens)
- Ever been pregnant
- Had certain disease, such as lupus, lymphoma or certain types of cancer
There are also other types of antibodies which are rare but important for blood typing. Examples of these antibodies are: Anti-C, Anti-Kell, Anti-Jka, Anti-Fyb, Anti-s, and so on. These antibodies may develop naturally, from pregnancy, or from a blood transfusion.
Yes. The antibodies formed to protect you against Rh-positive red blood cells can pass to the baby you are carrying. They attack and destroy the baby’s Rh-positive red blood cells, causing anemia (low red blood cell count), jaundice, and in severe cases, heart failure. This condition is known as hemolytic disease of the newborn.
Hemolytic Disease of the Newborn usually does not affect the mother’s first baby, but once she has produced Rh antibodies, all future Rh-positive babies are at risk. Rh Immune Globulin is given to prevent the production of these antibodies.
Hemolytic disease of the newborn (HDN) is an alloimmune condition that develops in a fetus, when antibodies that have been produced by the mother and have passed through the placenta include ones which attack the red blood cells in the baby’s circulation. The mother’s immunization results in the destruction of fetus’ red blood cells (hemolysis), accumulation of metabolites of red blood cell in tissues, such as skin (jaundice) or brain (kernicterus).
During the birthing process, blood cells from the unborn child can escape into the mother's bloodstream. These cells are recognized as foreign if they are a different blood type from the mother and a natural rejection process will ensue with the formation of antibodies. The process is known as red cell alloimmunization. This event typically occurs after the delivery of a baby at the end of pregnancy, but other pregnancy-related events such as elective abortion or spontaneous miscarriage can result in antibody formation. Although the pregnancy in which the alloimmunization first occurs results in an unaffected child, future children are at substantial risk. In these subsequent pregnancies, newly formed antibodies in the pregnant patient can cross to the unborn child and attach to its red blood cells producing a low blood count (anemia) and in the worst case scenario, fetal death. In general, the fetus of each subsequent pregnancy exhibits more severe effects than in the previous pregnancy. The fetal and newborn effects of red cell alloimmunization are known as hemolytic disease of the newborn.
Data from the Centers for Disease Control (CDC) indicate that the incidence of hemolytic disease of the newborn is approximately one case per 1000 live born infants.
Medicine is available to prevent Rh disease. RhO (D) immune globulin should be administered to the Rh-negative woman with a Rh-positive partner any time there is a chance fetal cells may enter the
pregnant woman's circulation. Such events include threatened miscarriage, spontaneous miscarriage, ectopic pregnancy, chorionic villus sampling or amniocentesis performed for genetic indications, and abdomen trauma. RhO (D) immune globulin should be administered routinely at 28 weeks of pregnancy and after the delivery of an Rh-positive infant.
If given correctly, this medication is more than 99% effective in the prevention of Rh disease. RhO (D) immune globulin immune globulin is only effective in preventing Rh disease; it is not effective in preventing worsening disease once alloimmunization has occurred.
It is estimated that each donation of Anti-D / Rh= plasma produces 36 RhO (D) immune globulin doses, enough to safeguard 18 births.
Once you have an antibody in your blood system, you will always have the antibody. The strength of the antibody will decrease in time, but it will always be present in your blood.
